Prepare for Your CHA
Cultivating and sustaining effective community partnerships is crucial to ensuring your CHA has a positive impact. The CHA allows hospitals, stakeholder organizations and community members to collaboratively identify and prioritize community health needs; assessing strengths and weaknesses should be part of this process. It is a tool for leveraging hospital and community assets to meet those needs. CHA findings illuminate the path for partners to implement strategies that measurably improve community health. A successful CHA collaboration helps both hospitals and communities reach their individual and shared goals.
View additional resources to futher your CHA journey.
Learn More About Hospital, Health System and Community Goals
Hospital/Health System Goals
- A clearer understanding of the community served by your hospital, including specific health issues, their underlying causes and the availability of resources and assets to address them.
- Increased trust between community and hospital, leading to increased collaboration around priority issues.
- Greater community collaboration toward shared stewardship of and commitment to community health.
- Strengthened relationships with individuals and organizations that are assets for improving community health.
- Healthier communities in which individuals have access to preventive care and seek care at the appropriate level.
- Increased understanding of the hospital’s role and capacity to impact health issues.
Community Goals
- A clearer understanding of the hospitals and health care organizations that serve your community, including the availability of resources and assets to address needs.
- Increased trust between community and hospital, leading to increased collaboration around priority issues.
- Self-determination of the community’s future health and well-being.
- Consideration of residents’ day-to-day lives, experiences and knowledge of community health care improvement.
- Health care solutions and strategies that align with community values.
- Strengthened relationships with individuals and organizations that are assets for improving community health.
- Continued involvement and investment in the short-term and long-term success of the CHA process and any subsequent community coalitions or collaborative improvement efforts.
Tips
Leverage the assessment for advancing community transformation.
The Assessment for Advancing Community Transformation (AACT) may be a helpful aid in preparing for the CHA. It's a self-directed tool to help any partners and collaborators understand how far along they are in their journey toward health transformation and what areas can be strengthened to help them go further.
Effective Community Partnerships
Taking a model off the page and putting it into practice is not easy. The same applies to effectively engaging the community in developing a CHA. Going beyond outreach to true, enduring community partnership requires an ongoing concerted effort, plus time to cultivate and sustain the relationship. Hospitals foster a sense of coproduction and joint ownership of the assessment by inviting the community to be a part of the process throughout.
The AHA co-developed the Partnership for Public Health Crosswalk with the Centers for Disease Control and Prevention, the National Association of County and City Health Officials, and the CDC’s Center for State, Tribal, Local and Territorial Support.
Regional collaborators collect data and may conduct regular assessments of the community and the specific populations they serve. Local or state public health agencies offer great value as CHA partners. The more aligned a hospital can become with the community by gathering these multiple perspectives, the stronger the opportunity will be for a unified assessment of community needs.
Input Collection
You can gain perspectives on your defined CHA region by soliciting input from a wide range of voices — residents as well as stakeholders. These collaborators include local health departments, agencies on aging and information/referral services such as 211. Other critical voices include organizations that support social connectedness and are pillars of the community. These include block clubs, neighborhood coalitions, churches, businesses, civic and social clubs, local online communities and funders.
Asset Mapping
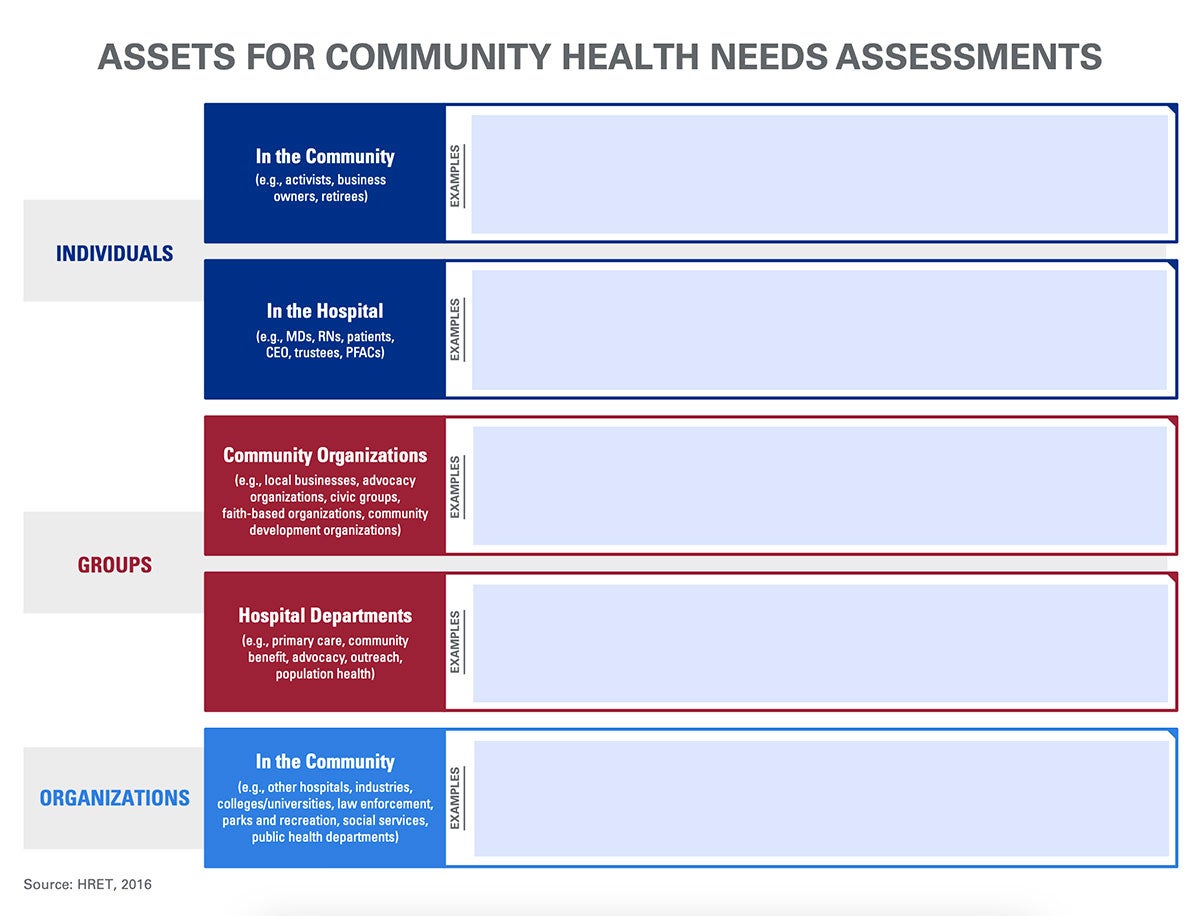
The process of asset mapping emphasizes individuals, networks and organizations in the community that can be engaged to improve community health and inform a hospital’s decisions about services. This process can enlighten unexpected stakeholders or partners.1
Asset-based framing is the practice of highlighting a community’s strengths, skills and resources instead of focusing on its problems or weaknesses. This approach is the preferred standard because no community appreciates being defined by its challenges or vulnerabilities. Instead, asset-based framing emphasizes the positive aspects that can empower and inspire growth.
Assets
Types of assets include the following:
- Human: An organization’s staff, board of directors, programs, membership and target population, including individual expertise, talent, training and skills.
- Physical: A geographic location that is accessible to the target population and provides public space and meeting rooms.
- Informational: Formal and informal networks of communication and participation in formal and informal associations.
- Political: Constituencies of elected officials and public and private institutions that advocate for resources and policy changes.
- Existing intervention: Initiatives that are already occurring in the community.
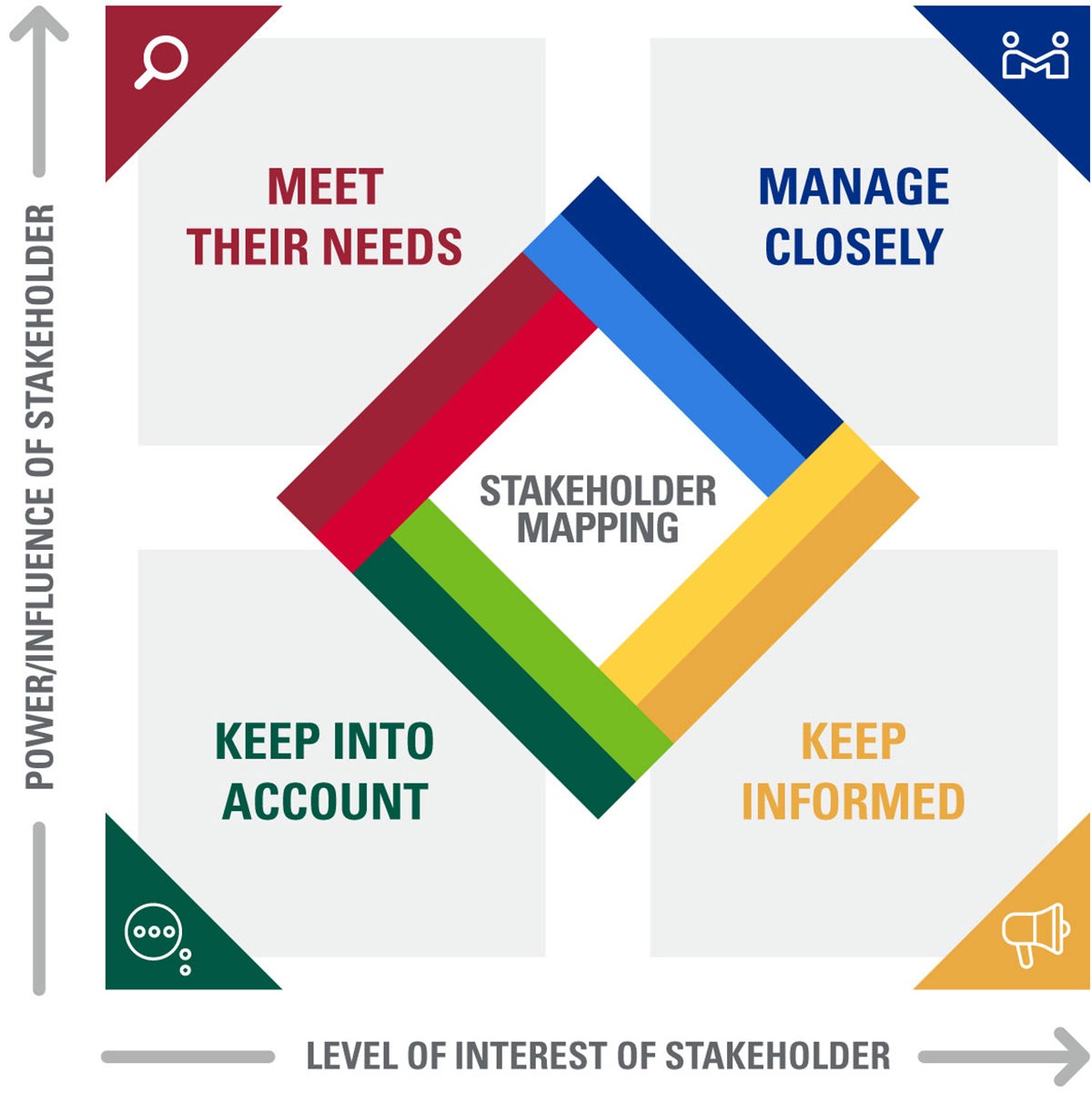
Mapping community assets early in the process can draw unexpected stakeholders or new partners to engage in the CHA. In recent years, asset mapping has evolved to bring deeper insight to community health initiatives, particularly to reduce disparities in heRalth outcomes. Specifically, stakeholder and/or power mapping have emerged as powerful tools that look at not just who or what the assets are but how much a stakeholder group values a specific endeavor, how central they would be to its successful implementation and how much power or control they might have over its outcomes. Borealis offers more information on stakeholder mapping as represented in Figure 3.
 >
> Strategic Timing
Even before you articulate key questions and types of data to collect, engage your stakeholders. Their lived experience can enrich and inform your process from the start. Emphasize cocreation instead of the more traditional mode of presenting a: a plan, and then ask for input.
Respectful, Realistic Expectations
Community engagement is an ongoing and thoughtful process, always balanced by a hospital’s respect for community leaders and their already busy, committed schedules. In advance, ask community members about reasonable expectations for their involvement. Coordinate your efforts with other organizations so that the same individuals are not tapped for multiple assessments. Be intentional about how and on what you ask for input. Lastly, consider using virtual meeting platforms when appropriate, to limit the burden of travel, child care and other considerations.
Accountability
Keep in mind that your community partners view the CHA as one aspect of an ongoing relationship. Be accountable and responsible to your stakeholders, who contribute time and energy to the CHA process and to other projects you share. Be sure to provide frequent updates and invitations for input and shared decision-making. Your accountability will best ensure these stakeholders will be there for the next CHA and for other partnerships, as well.
Transparent Communication
Be clear and appropriately transparent about capacity and objectives for your work together. It is important to anticipate financial and capacity limits in your opening conversations. Going beyond requirements can be possible even in resource-constrained settings through partnership, hospital employee volunteerism, providing technical support and bringing community assets to the table. Consider other organizations and individuals out there that are invested in areas of focus and could contribute – Invite these players to participate in your CHA process.
Resources
The Community's Strengths
Start by mapping the community’s strengths, and then build toward consensus on priority areas that can best be addressed through these assets. Individuals, groups and organizations to inventory include:
- Community members, including but not limited to those participating in community-based initiatives.
- Government, public, private and philanthropic institutions.
- Representatives of the local economy and workforce development
- Holders of physical spaces where the community might be engaged (e.g., community gardens, libraries).
- Associations (neighborhood, tenant, legal, advocacy, faith-based, etc.).
Template for a Community Asset Map